SAFE HEARTS PLAN – A positive yet insufficient step towards improving cardiorenal health
The European Kidney Health Alliance (EKHA) commends the European Commission’s Safe Hearts Plan for its ambitious approach to tackling cardiovascular diseases (CVDs) and related comorbidities, including kidney disease. Recognising the heart-kidney link across the disease spectrum is a positive step, but the attention remains far too modest compared to the scale of the challenge.
Missing kidney disease targets
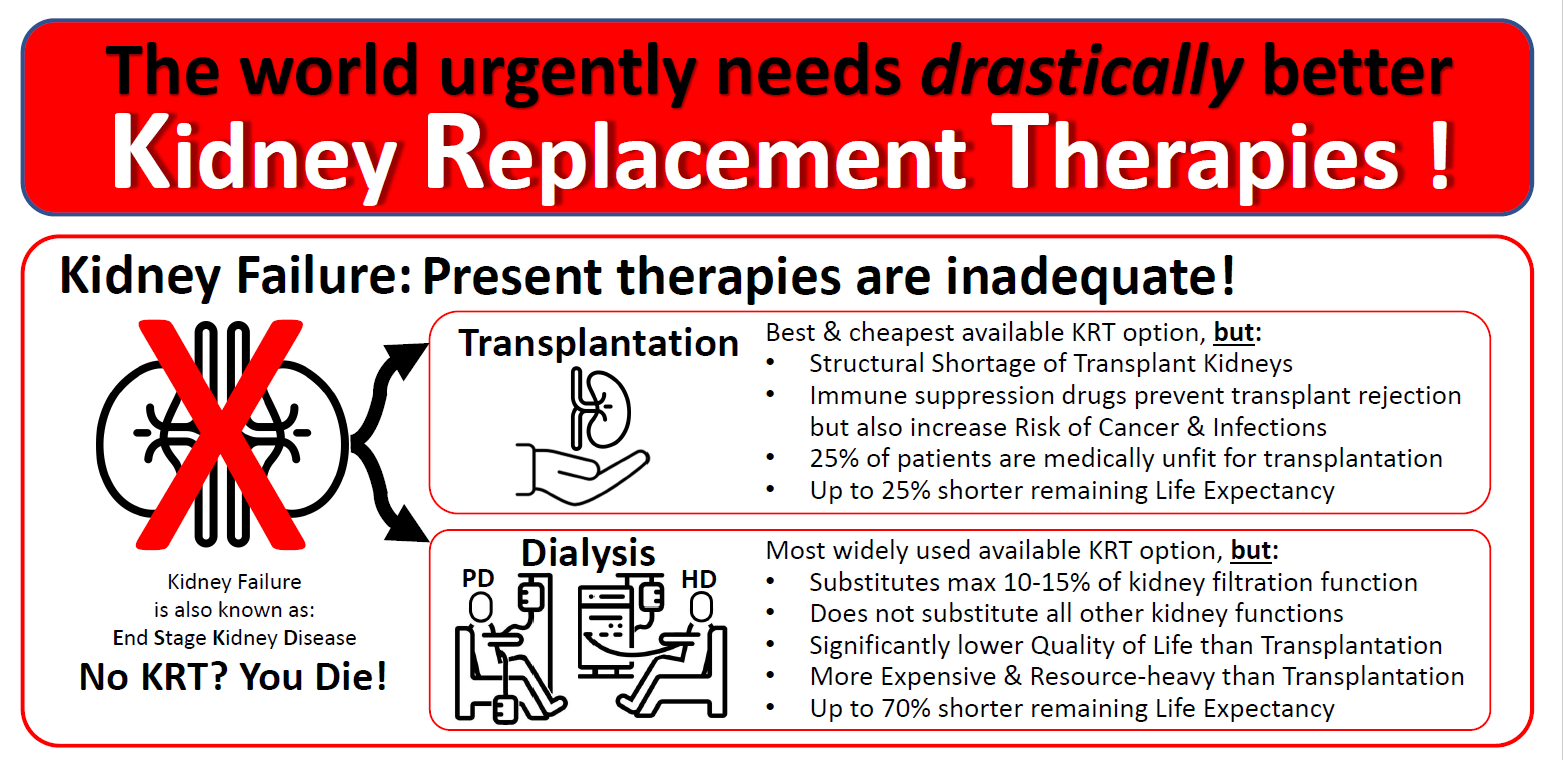
While EKHA welcomes the inclusion of targets for CVDs, hypertension, diabetes and obesity by 2035, the absence of kidney disease targets remains a significant concern. Chronic kidney disease (CKD) sits at the crossroad of all these conditions and its prevalence is increasing: up 44% since 1990, now affecting 10% of the population, and projected to become the third leading cause of death by 2050. Downplaying this escalating threat will only slow progress in combatting CVDs.
Screening and early detection: more should be done
The mention of CKD as an additional disease to be screened alongside diabetes and obesity marks important progress. However, the proposed EU protocol on health checks leaves unclear how this will be integrated. To effectively address the early-detection gaps, the health checks must adopt a holistic approach to identifying cardio-kidney-metabolic diseases, for example by encouraging Member States to upscale Albuminuria screening – a proven biomarker for kidneyheart risk that remains underused in Europe.
Unaddressed gaps in kidney disease data
While the plan mentions the data gaps in CVD, diabetes, hypertension and obesity, it overlooks similar shortcomings for CKD. Most Member States lack comprehensive, standardised national registries for CKD and datasets overall remain fragmented across the EU. This lack of harmonised data significantly constrains clinical research, the development of personalised care models, and evidence-based policymaking. The proposed incubator for innovation and integration of AI and digital technologies must also address CKD data limitations.
Positive advances on prevention, cardiorenal research and integrated care models
Prevention is the most cost-effective way to tackle NCDs. Initiatives such as providing consumer information on food processing, introducing levies on ultra-processed food, high-fat, salt food and drinks, as well as modernising the EU tobacco control legislation are all important public health measures that must remain ambitious to effectively reduce the burden of CKD and CVDs.
Equally relevant is the flagship initiative to advance research on cardiovascular, metabolic and renal disease under the European Partnership for Personalised Medicine – a crucial step to address research gaps on a critical yet under-recognised condition in Europe.
Lastly, the plan promotes integrated care models for individuals living with CKD, diabetes and CVDs, which represents a step forward. The proposed Council Recommendation on
personalised treatment and monitoring of CVDs must fully incorporate the benefits of these models to enable better coordination across primary care and medical specialties, improve patient outcomes and reduce duplication of services.
As it stands, the Safe Hearts Plan is a welcome first step, but also a missed opportunity to deliver a comprehensive approach to cardio-renal-metabolic health. Neglecting this interconnection is neither scientifically sound nor cost-effective for healthcare systems. We urge the Council of the EU and the European Parliament to address these shortcomings in the upcoming discussions and implementation activities to ensure that the Safe Heart Plan delivers meaningful change for all patients with metabolic disorders across the EU.
Prof. Valerie Luyckx, EKHA Co-President
Prof. Michel Jadoul, EKHA Co-President